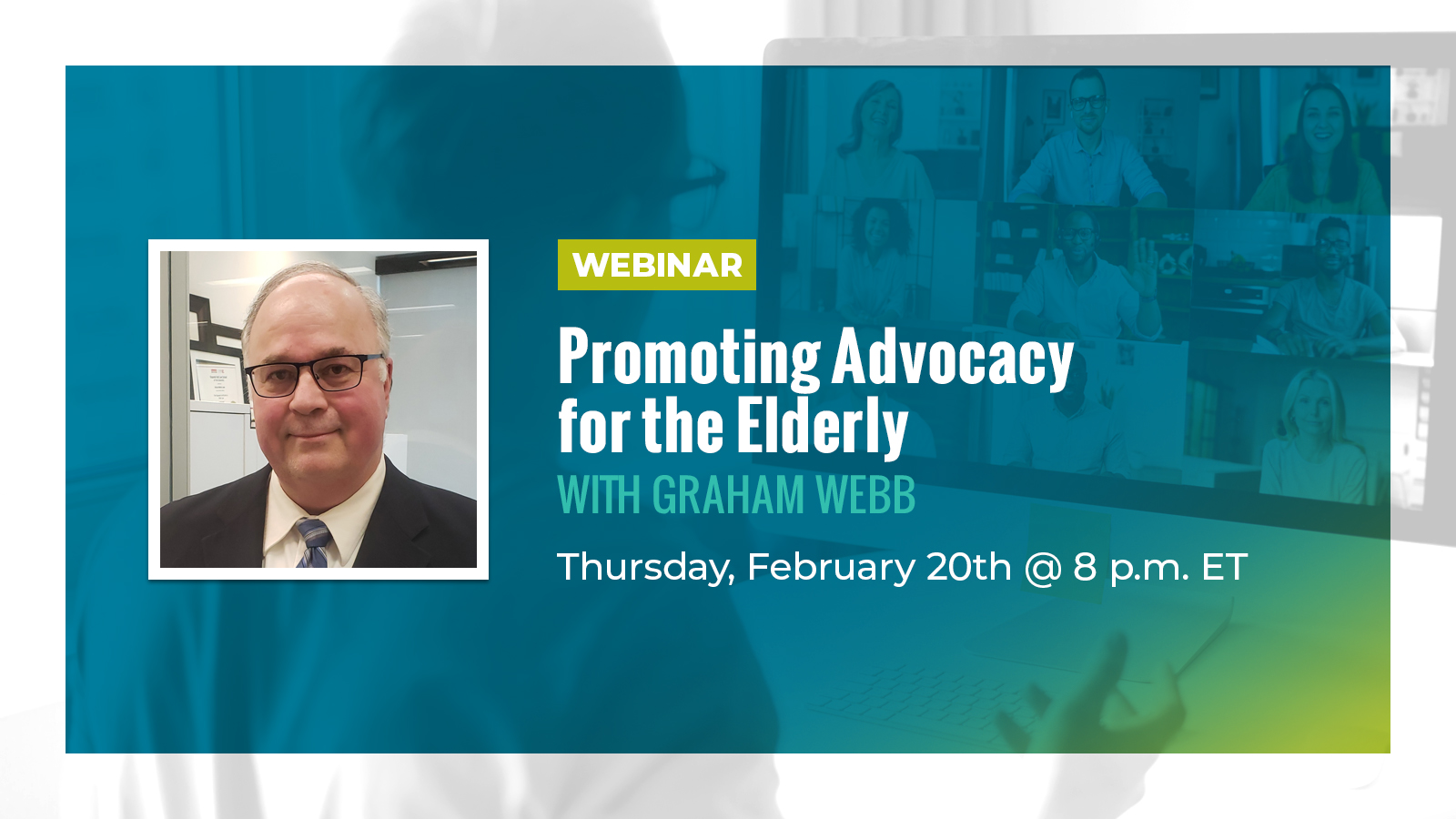
Brief Submitted to the Senate Committee Studying Bill C-7: An Act to Amend the Criminal Code (medical assistance in dying)
Since Bill C-7 will primarily affect people who are vulnerable and marginalized, I would like to begin this brief by sharing a vignette from a recent interaction between one of our physician members and a patient.
What are your thoughts on killing the elderly?” She asked me frankly. “What an introduction,” I thought. I never had someone open our first meeting with that kind of question. I paused for a moment and responded, “I don’t kill my patients. You can feel confident that I will provide the best possible care to your aunt, and I am trained to provide palliative care at the end of life.” She was relieved. Her aunt was relieved. Trust was established. Our caregiving relationship began.
Physicians who belong to our organization professionally adhere to the time-honoured Hippocratic medical tradition. Our physicians not only have clinical practices but also work in hospitals and retirement homes providing care to some of the most frail and vulnerable members of our society. They see people who rely on an army to live. They see people suffering from mental illnesses, physical ailments, and chronic disease. Despite all of the morbidity they see daily, they also see these older adults finding joy in small gains, appreciating the life they are living, and redefining hope in their lives. These older adults are one group who is most at risk of prematurely losing their lives because of unnecessary changes to MAiD contemplated by Bill C7.
Our members report that the patients they are meeting daily and the families they interact with are losing trust in our healthcare system and in healthcare providers. When the patient-provider relationship erodes, it is impossible to provide quality care. Working with older adults has exposed many instances where requests for medical assistance in dying (MAiD) were actually indicative of a need for palliative care.
Because I think they are illustrative, I want to share some patient stories told to me by member physicians:
This story is from a physician who specializes in Care for the Elderly.
“One patient I encountered did not see the reason she should keep living as her relationship with her children was eroding and she was experiencing unbearable pain. Providing her with quality palliative care after our first meeting greatly improved her pain levels. Several counselling sessions about her family life allowed her to gain the confidence to rebuild a relationship with her son. She needed support, a listening ear, and good medical management to live a full life to the end instead of a physician who offered to end it all before exploring further. She died peacefully and naturally three months later after enjoying an ice cream every day and a newly rebuilt relationship with her son.”
There is a legacy left at the individual level and a wider social good. That restored relationship is carried through in her son’s life and its positive effect will cascade to many others.
Another story from a psychiatrist
“I spent over 4 hours on Tuesday night talking a chronically suicidal patient out of jumping off a bridge after multiple suicide attempts in the past two months, and convinced her to meet me at the hospital to get treatment that she needed to stay stable. A phone conversation that began with her at the bridge saying: “I just want to die”, ended 5 hours later, not with tragedy, but thankfully with a renewed sense of hope in the patient, and a desire to try again to work together toward a better path.
At the hospital, she cried through her tears: “Doctor, thank you for not giving up on me.” And when I asked her after, as she contemplated ending her life after she had already called other supports and did not find them to be helpful, what stopped her from jumping? She looked directly into my eyes and exclaimed: “YOU! When you called me! THAT’s what stopped me!”
The Royal College of Physicians and Surgeons says that the excellent physician is a Health Advocate for their patient so that they are not “being disadvantaged by, for example, race, ethnicity, religion, gender, sexual orientation, age, social class, economic status, or level of education.”
Physicians fight for their patients’ lives everyday. They make tremendous personal sacrifices and place all of their skills at the service of their patients. They must be allowed to apply the standard of care and that takes time. It takes time to establish goals of care in collaboration with the patient and their families. It takes time to establish a patient-centred management plan. It takes time to get to the root of the psychosocial needs of the patient.
As it now stands Bill C-7 will undermine the physician-patient relationship. The trust that is essential for good medical care will disappear. The healthcare system will be fundamentally altered, and individuals will be disadvantaged.
It is imperative Bill C-7 be amended to protect vulnerable populations including older
adults. Specifically safeguards such as the following are essential:
- two independent witnesses,
- a 10-day reflection period to help prevent someone’s worst day from becoming their last day, and
- contemporaneous consent.
MAiD has been deemed an essential service in Canada. Currently, palliative care is not
an essential service. Palliative Care needs to be deemed an essential service under the Canada Health Act. This would ensure all Canadians have access to compassionate end of life care that allows them to both live and die with dignity.
When physicians are allowed to act with compassion and care, there are societal benefits that reach beyond the individual patient. Bill C-7 as it now stands will seriously undermine the role of the physician as healer. The ramifications for the medical profession and society are far-reaching.
We ask the Senate to ensure there are adequate safeguards under Bill C-7. Let this be the legacy of your consideration of this complex and challenging matter.
You Might Also Like
Follow US: